The Nipah virus (NiV) is a formidable foe in the world of emerging infectious diseases, posing a significant public health threat with its high fatality rate and potential for widespread outbreaks. As of 2025, understanding NiV is more crucial than ever, given its zoonotic origins and the complexities involved in its detection, treatment, and prevention. This comprehensive guide will delve deep into the Nipah virus, offering an in-depth look at its history, transmission, symptoms, global impact, and the latest scientific advancements in combating this elusive pathogen. Our aim is to equip you with robust, up-to-date knowledge that could be vital in a world increasingly challenged by novel viruses.
What is the Nipah Virus (NiV) and Why is it So Concerning?
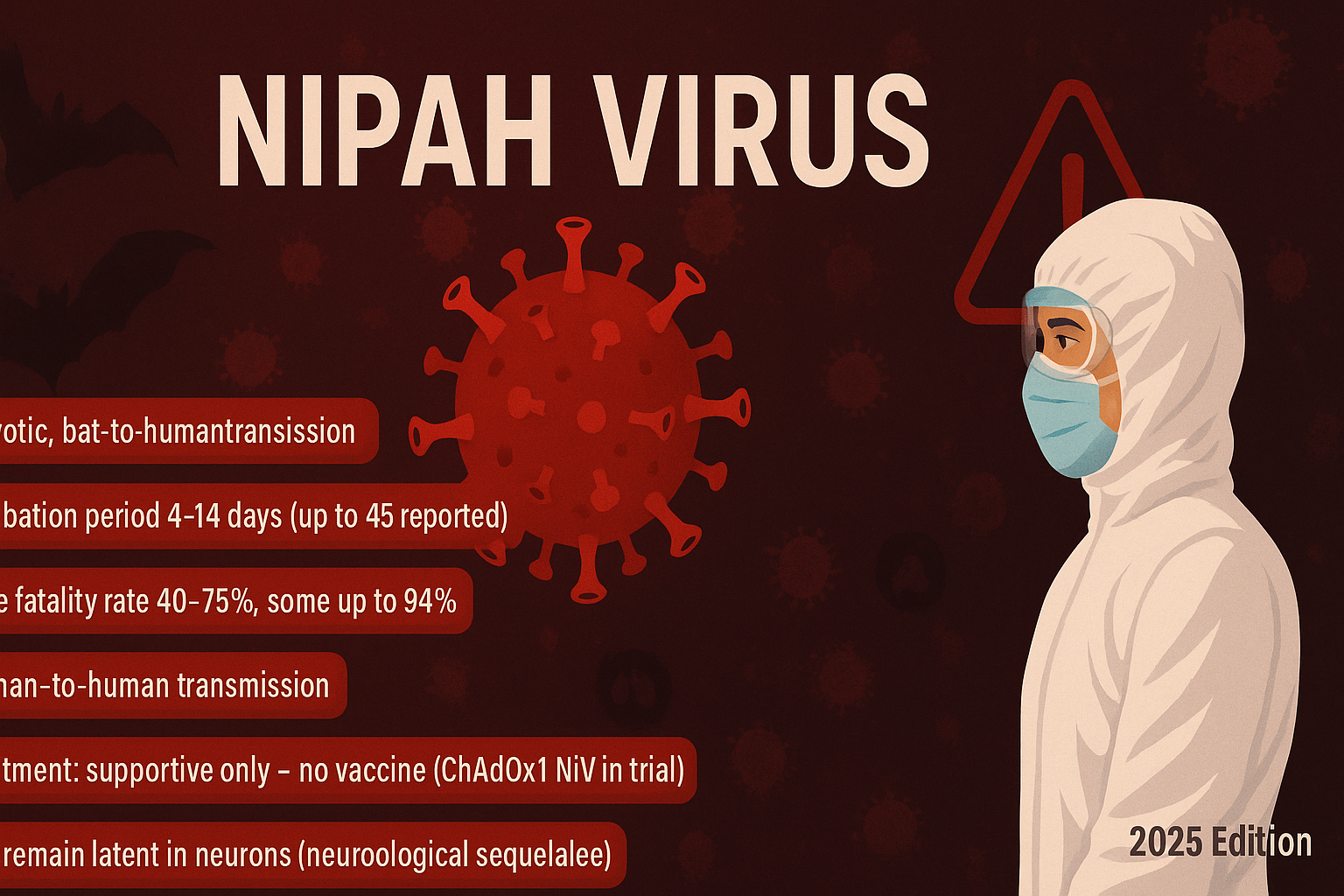
The Nipah virus (NiV) is a highly pathogenic paramyxovirus that causes severe encephalitis and respiratory illness in humans. First identified in 1998 during an outbreak among pig farmers in Malaysia and Singapore, the virus quickly garnered international attention due to its rapid spread and devastating impact. The primary concern surrounding NiV stems from its high case fatality rate, which can range from 40% to 75% depending on the outbreak and region, and its potential to cause large-scale epidemics. Furthermore, NiV is a zoonotic virus, meaning it can transmit from animals to humans, primarily through infected fruit bats (Pteropus genus) and pigs, but also directly from human to human contact. This complex transmission pathway makes containment particularly challenging. The lack of a licensed vaccine or specific antiviral treatment for human NiV infection further amplifies its threat, highlighting the urgent need for continued research and public health preparedness.
The Origin Story: Where Did Nipah Virus Come From?
The Nipah virus takes its name from Sungai Nipah, a village in Malaysia where it was first isolated. The initial outbreak in 1998-1999 primarily affected pig farmers. Investigations revealed that the virus had jumped from fruit bats (Pteropus species), which are natural reservoirs for NiV, to pigs, and subsequently to humans. The deforestation and agricultural expansion in the region brought bats into closer contact with pig farms, facilitating the spillover event. Since then, subsequent outbreaks have occurred in Bangladesh and India, demonstrating slightly different epidemiological patterns. In these regions, human infection has largely been linked to consuming raw date palm sap contaminated with bat excreta or saliva, and direct human-to-human transmission has also been a significant factor. This geographical shift and variation in transmission routes underscore the adaptable nature of the virus and the diverse ways it can emerge.
How Does Nipah Virus Spread? Understanding Transmission Pathways
Understanding the multifaceted transmission pathways of the Nipah virus is crucial for effective prevention and control. NiV primarily spreads through three main routes:
Zoonotic Transmission: From Animals to Humans
The most common initial route of infection is zoonotic transmission, primarily from infected animals to humans.
- Fruit Bats (Pteropus genus): These are the natural hosts of the Nipah virus. Bats can shed the virus through their urine, feces, saliva, and birthing fluids. Humans can become infected by consuming fruits or date palm sap contaminated with bat excretions, or by direct contact with infected bats or their habitats.
- Pigs: In the initial Malaysian outbreak, pigs served as an intermediate host, amplifying the virus and transmitting it to humans. Pigs can become infected by consuming contaminated fruits or through contact with infected bats. Infected pigs can then transmit the virus to humans through direct contact with their secretions or tissues, especially during slaughtering or handling.
Human-to-Human Transmission: The Spreading Threat
While not as common as zoonotic transmission in the initial stages of an outbreak, human-to-human transmission has been a significant factor in some outbreaks, particularly in Bangladesh and India.
- Close Contact: The virus can spread through close contact with an infected person’s bodily fluids, including respiratory droplets, urine, and blood. Healthcare workers and caregivers are at higher risk if proper infection control measures are not followed.
- Contaminated Surfaces: Although less documented, the possibility of indirect transmission through contact with contaminated surfaces or objects cannot be entirely ruled out, emphasizing the need for robust hygiene practices.
Recognizing the Signs: Symptoms of Nipah Virus Infection
The symptoms of Nipah virus infection can vary widely, ranging from asymptomatic to severe encephalitis and death. The incubation period typically ranges from 4 to 14 days, though it can extend up to 45 days.
Early Symptoms: Mimicking Common Illnesses
Initial symptoms often resemble those of a common flu, making early diagnosis challenging. These can include:
- Fever: Often high-grade and sudden onset.
- Headache: Severe and persistent.
- Muscle Pain (Myalgia): Generalized body aches.
- Sore Throat: Discomfort when swallowing.
- Vomiting and Nausea: Gastrointestinal distress.
Progressing to Severe Illness: Neurological and Respiratory Complications
As the disease progresses, patients can develop more severe and life-threatening complications, particularly affecting the respiratory and neurological systems.
- Acute Encephalitis: This is the most serious manifestation, characterized by:
- Drowsiness and Disorientation: Confusion and difficulty concentrating.
- Seizures: Uncontrolled electrical activity in the brain.
- Coma: A state of prolonged unconsciousness.
- Brainstem Dysfunction: Leading to abnormal posturing and difficulties with vital functions.
- Acute Respiratory Syndrome (ARS): Some patients may develop severe respiratory problems, including:
- Cough: Persistent and sometimes productive.
- Shortness of Breath (Dyspnea): Difficulty breathing.
- Acute Respiratory Distress Syndrome (ARDS): A severe lung condition that prevents enough oxygen from getting into the blood.
A subset of patients who recover from acute encephalitis may experience relapsed encephalitis or delayed-onset encephalitis months or even years after the initial infection, highlighting the long-term neurological sequelae of NiV.
Global Impact and Outbreak History: Where Has NiV Struck?
While the initial Nipah virus outbreak was confined to Southeast Asia, its re-emergence and subsequent outbreaks in different geographical locations underscore its global public health significance.
The Malaysian Origin (1998-1999)
The first major outbreak in Malaysia and Singapore resulted in over 265 reported cases and 105 deaths. This outbreak led to the culling of over a million pigs to control the spread, causing significant economic disruption to the pig farming industry.
Persistent Threat in Bangladesh and India (Since 2001)
Since 2001, Bangladesh has experienced nearly annual outbreaks of Nipah virus, predominantly in the central and northern districts. These outbreaks often coincide with the date palm sap harvesting season. In India, outbreaks have been reported in the states of West Bengal and Kerala, with the most recent significant outbreak in Kerala in 2018 and subsequent smaller clusters. The recurring nature of these outbreaks, often linked to distinct transmission routes (like contaminated date palm sap), emphasizes the need for tailored public health interventions.
Table 1: Key Nipah Virus Outbreaks (Selected, 1998-2025)
Note: Data for recent years (2019-2025) reflects sporadic, localized outbreaks. Case and death numbers are approximate and subject to change based on official reports.
Preventing the Unseen: Current Control and Prevention Strategies
Given the absence of a specific treatment or vaccine, prevention and control are paramount in managing Nipah virus outbreaks.
Public Health Interventions: Community-Level Protection
- Awareness Campaigns: Educating communities, especially in endemic areas, about the risks and preventive measures is crucial. This includes advising against consuming raw date palm sap, thoroughly washing fruits, and avoiding contact with sick pigs or bats.
- Surveillance: Robust surveillance systems are essential for early detection of cases in both human and animal populations. This allows for rapid response and containment measures.
- Slaughterhouse Safety: Implementing strict biosecurity measures in pig farms and slaughterhouses can prevent zoonotic transmission from pigs to humans.
Personal Protective Measures: Shielding Yourself
- Hand Hygiene: Frequent and thorough handwashing with soap and water is critical, especially after contact with animals or potentially contaminated environments.
- Food Safety: Avoid consuming raw date palm sap. Thoroughly wash and peel fruits, especially those that may have been exposed to bat secretions. Avoid consuming fruits with signs of bat bites.
- Avoiding Contact with Bats and Sick Animals: Limit direct contact with fruit bats and their roosting sites. If working with livestock, especially pigs, use appropriate personal protective equipment (PPE).
- Infection Control in Healthcare Settings: Healthcare workers caring for NiV patients must adhere to strict infection control protocols, including wearing masks, gloves, gowns, and eye protection, to prevent human-to-human transmission.
The Race for a Cure: Research and Development in 2025
The scientific community is actively engaged in developing countermeasures against the Nipah virus, with significant progress being made in several areas by 2025.
Vaccine Development: A Glimmer of Hope
Several vaccine candidates are in various stages of preclinical and clinical development. These include:
- Subunit Vaccines: Utilizing specific viral proteins to trigger an immune response.
- Viral Vector Vaccines: Using a modified, harmless virus to deliver NiV genetic material to stimulate immunity.
- mRNA Vaccines: Leveraging messenger RNA technology, similar to some COVID-19 vaccines, to produce viral proteins and induce an immune response.
While no licensed human vaccine is yet available, the ongoing research offers promising prospects for future protection, particularly for high-risk populations like healthcare workers and those in endemic regions.
Antiviral Therapies: Targeting the Virus
Research into antiviral drugs capable of inhibiting NiV replication is also ongoing. While ribavirin was used empirically in earlier outbreaks, its efficacy remains unproven. Newer compounds are being investigated for their potential to block various stages of the viral life cycle. Monoclonal antibodies are another promising avenue, offering a targeted approach to neutralize the virus.
Diagnostic Tools: Rapid and Accurate Detection
Accurate and rapid diagnostic tests are vital for early detection and containment. Advancements in molecular diagnostics, such as real-time RT-PCR, allow for quicker and more reliable identification of the virus in patient samples. Development of point-of-care tests is also a priority to facilitate rapid diagnosis in resource-limited settings.
Pro Tips for Staying Safe from Emerging Zoonotic Threats
Staying informed and proactive is your best defense against emerging zoonotic diseases like Nipah virus. Here are some expert tips:
- Be Mindful of Local Food Practices: If traveling to regions where NiV is endemic, exercise caution with local food and drink, especially fresh fruit and unpasteurized date palm sap.
- Practice Excellent Hygiene: Regular and thorough handwashing is your first line of defense against many infectious agents.
- Avoid Contact with Wild Animals: Steer clear of bats and other wild animals, especially if they appear sick or are in unusual locations.
- Support Sustainable Practices: Advocate for and support initiatives that promote sustainable agriculture and prevent deforestation, which can reduce human-wildlife encroachment.
- Stay Informed and Consult Experts: Follow advisories from reputable health organizations like the WHO and local health authorities. If you experience symptoms after potential exposure, seek medical attention immediately and inform your healthcare provider about your travel history.
- Advocate for Research and Preparedness: Support efforts in vaccine development, antiviral research, and strengthening global health preparedness for future outbreaks.
Frequently Asked Questions About Nipah Virus
What is the primary reservoir for Nipah virus?
The primary natural reservoir for the Nipah virus is fruit bats of the Pteropus genus, also known as flying foxes. These bats carry the virus without showing signs of illness and can shed it through their bodily fluids, contaminating fruits and other food sources.
Is there a vaccine or specific treatment for Nipah virus?
Currently, there is no licensed vaccine or specific antiviral treatment available for Nipah virus infection in humans. Treatment is primarily supportive, focusing on managing symptoms and complications such as encephalitis and respiratory distress. Research and development for both vaccines and antiviral drugs are actively ongoing.
How can I protect myself from Nipah virus infection?
Key protective measures include avoiding contact with sick pigs and bats, not consuming raw date palm sap, thoroughly washing and peeling fruits before consumption, and practicing good personal hygiene, especially handwashing. In healthcare settings, strict infection control measures are crucial.
Can Nipah virus spread from person to person?
Yes, human-to-human transmission of Nipah virus has been documented, particularly in South Asian outbreaks. This typically occurs through close contact with an infected person’s bodily fluids, such as respiratory secretions, urine, or blood. Healthcare workers and caregivers are at higher risk.
What are the long-term effects of Nipah virus infection?
Patients who survive Nipah virus encephalitis may experience long-term neurological sequelae, including personality changes, seizures, and persistent neurological deficits. Some individuals may also develop relapsed encephalitis or delayed-onset encephalitis months or years after the initial infection.